- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board

Early Warning Signs of Multiple Sclerosis (MS)
Early warning signs, most common symptoms.
- Males vs. Females
Frequently Asked Questions
While no two people experience multiple sclerosis (MS) the same way, some symptoms tend to crop up earlier in the disease course than others. These symptoms may serve as warning signs of the disease, potentially allowing you or a loved one to receive a diagnosis of MS sooner than later.
In multiple sclerosis, your immune system goes awry and damages the fatty covering ( myelin ) that insulates nerve fibers within your central nervous system (CNS). Your CNS consists of your brain, spinal cord, and the optic nerves of your eyes.
As a result of myelin damage, nerve signals cannot be transmitted rapidly or efficiently between the CNS and the rest of your body. This can lead to various symptoms like blurry vision, pain, abnormal sensations, and muscle weakness, among many others.
This article reviews some of the common early symptoms and signs of MS. It also gives a brief overview of differences of MS between males and females and how MS is diagnosed.
peakSTOCK / Getty Images
Two phenomena—clinically isolated syndrome and optic neuritis—may serve as early warning signs of MS. People who experience one (or both) of these may or may not go on to develop MS.
Clinically Isolated Syndrome
Clinically isolated syndrome (CIS) refers to a person's first-time episode of neurological symptoms caused by inflammation and damaged myelin in the CNS.
As an example, a patient diagnosed with CIS may experience numbness and tingling in their legs. This would be accompanied by magnetic resonance imaging (MRI) findings that reveal damage to the CNS.
CIS is followed by a recovery period where the symptoms improve or completely go away.
Difference Between CIS and MS
The key difference between CIS and MS is that CIS is diagnosed after a person experiences one episode of neurological symptoms. MS can only be diagnosed when a person has experienced more than one episode of neurological symptoms.
Optic Neuritis
Optic neuritis —inflammation of one of your two optic nerves—is a common first presentation of MS. In fact, CIS may be diagnosed from an attack of optic neuritis.
Your optic nerve delivers messages to your brain about what your eye sees. When the myelin covering the optic nerve is damaged, signals related to sight are interrupted.
The common symptoms of optic neuritis include pain with eye movements, blurry or "foggy" vision, and seeing colors less vividly. Vision symptoms usually improve and fully recover within three to five weeks. That said, up to 10% of patients may experience long-term vision problems.
Even though the symptoms of MS vary in type, severity, and duration, there are some that are more common than others. The following is a brief snapshot of such symptoms:
Vision Problems
Besides optic neuritis, other common vision problems seen in MS are:
- Nystagmus is uncontrolled, jerking movement of the eyes, sometimes referred to as "dancing eyes." This symptom is caused by damage to the area of the brainstem that controls eye movements.
- Diplopia (double vision) is uncoordinated eye movements that cause you to see double. This symptom results from damage to the nerves that control your eye muscles.
Muscle Spasms
Muscle spasms are common in MS and are primarily caused by damaged myelin in the nerves that innervate or connect to your muscles. As a result of disrupted nerve signals, your muscles cannot relax properly. This causes muscle stiffness and/or a tightening, cramping, or heavy sensation in the affected muscle(s).
The legs are most commonly affected by spasms, but they can occur anywhere in the body. Muscle spasms also tend to be asymmetric, meaning they are more likely to happen on one side of the body versus both sides.
Nerve fiber damage in MS causes neuropathic pain , which is associated with burning, stabbing, sharp, itching, or squeezing sensations. This type of pain is associated with disability, depression, and fatigue in MS.
Specific types of neuropathic pain that may be early signs of MS include:
- Lhermitte's sign is a sensation of electricity that runs down your spine when you touch your chin to your chest. In MS, it's caused by damage to nerve fibers in your upper spine.
- MS hug is a tightening sensation around the chest and ribs caused by damage to the nerve fibers in your spine.
- Trigeminal neuralgia is an electric-shock-like or stabbing pain in the face or jaw area that is caused by damage to the trigeminal nerve (the fifth cranial nerve ).
Fatigue and Weakness
MS fatigue is often felt both physically and mentally. Described by many as "having the flu," MS fatigue is not eased by sleep and tends to come on suddenly and worsen with heat and humidity.
The overwhelming exhaustion and depletion of energy seen with MS fatigue may arise from the disease itself and/or other factors like medications, sleep disorders, or depression.
Timeline of MS Fatigue
Fatigue can occur at any time during the course of MS, and its development is not necessarily related to the progression of more objective neurological symptoms (e.g., walking problems).
Weakness is also common in MS and may arise from damage to the nerve fibers in the CNS that normally control muscle movements. Lack of activity due to MS-related pain, fatigue, or other symptoms can also contribute to MS weakness.
Bladder and Bowel Problems
Bladder dysfunction is common in MS, affecting the majority of patients at some point in the course of their disease. Urinary symptoms as the first presentation of MS occur in around 3% to 10% of people.
Symptoms and signs of bladder dysfunction in MS vary from mild to severe. They may include:
- Urgency : Feeling like you have to urinate right away
- Hesitancy : Having trouble initiating urination or you cannot maintain a steady stream
- Nocturia : Having to urinate often at night
- Incontinence : Having an involuntary loss of urine control
Recurrent urinary tract infections may also be a sign of bladder dysfunction in MS.
Bowel problems are common in MS, with constipation being the most frequent complaint. Constipation can aggravate other MS symptoms including muscle spasms, pain, bladder dysfunction, and walking problems. It can also contribute to fecal incontinence, which is the loss of control of your bowels.
Depression and Emotional Changes
Depression is associated with constant sadness and a lack of interest in activities you once enjoyed. In MS, depression can occur at any time in the course of the disease, including early or later on.
Depression in MS may stem from a number of different factors, including:
- MS itself : Damage to the areas of the brain that regulate emotion
- Side effects of MS medications : For example, corticosteroids (used to treat MS relapses ) and interferon drugs (used as disease-modifying therapies )
- Stress associated with living with MS : Undergoing a new diagnosis, relapse, or major change in function.
Other common emotional symptoms in MS include grief, anxiety , irritability, and anger. Many of these emotions stem from the unpredictable nature of MS, and the physical and emotional impact the disease has on a person's life.
Presentation in Males vs. Females
Differences exist in MS in males and females. For instance, research has found that females are twice as likely to live with MS as males. Moreover, those diagnosed with primary progressive MS (PPMS) are more likely to be male.
What Is PPMS?
PPMS is characterized by worsening symptoms from the onset of the disease. People with PPMS do not experience relapses or periods of symptom improvement ("remission").
Experts haven't yet teased out fully why these differences between sexes exist. Sex hormones, pregnancy, social factors (delayed care-seeking behavior), and/or differences in genes or environmental exposures may be involved.
How MS Is Diagnosed
The diagnosis of MS is often challenging, considering the symptoms are so variable. In addition, symptoms early on can often be vague or mimic those of other conditions, such as systemic lupus erythematosus (SLE) (an autoimmune disease that can affect many body systems) or vitamin B12 deficiency .
A neurologist —a doctor who specializes in diseases of the nervous system—will use the following tools to confirm a diagnosis of MS:
- Your medical history and neurological exam
- The McDonald criteria (a set of guidelines that focuses on diagnosing MS by showing evidence of damage to the CNS at different dates and to different parts)
- Magnetic resonance imaging (MRI) of the brain and spinal cord (which uses strong magnets to produce detailed images)
- Laboratory tests, mostly to rule out other conditions
- Other tests, including a spinal tap (lumbar puncture) and evoked potential tests (which measure electrical activity of the nerves of the eye)
Even though no two people experience MS in the same way, there are some symptoms, including vision problems and sensory disturbances, that may serve as early warning signs of the disease. Other common symptoms of MS include fatigue, muscle spasms, pain, bladder problems, and constipation.
A Word From Verywell
If you are concerned that you may be experiencing possible symptoms of MS, schedule an appointment with your healthcare provider or a neurologist. Diagnosing and treating MS as early as possible is associated with better long-term outcomes .
Keep in mind that many symptoms of MS overlap with other common medical conditions. Be proactive and get checked out, but try not to worry yourself until you know more information.
Most people are diagnosed with MS between the ages of 20 and 50 years old. That said, MS can develop at any age, and symptoms may predate a diagnosis by years.
Yes. In fact, research suggests MS may have a prodromal ("very early") phase. This phase includes various nonspecific symptoms, like fatigue, depression, pain, and headache. These symptoms may precede an MS diagnosis by several years.
There is no blood test that can diagnose MS. If you or a loved one are being evaluated for MS, your neurologist will use a variety of diagnostic tools, including your medical history, neurological exam, an MRI, and various blood or spinal fluid tests.
MS occurs when your immune system mistakingly attacks myelin, a protective coating on your nerves. These attacks lead to inflammation in the brain and spinal cord. The inflammation shows up as "lesions" or "plaques" on an MRI .
National MS Society. Clinically isolated syndrome .
Kale N. Optic neuritis as an early sign of multiple sclerosis . Eye Brain. 2016;8:195–202. doi:10.2147/EB.S54131
Cavenaghi VB, Dobrianskyj FM, Sciascia do Olival G, Castello Dias Carneiro RP, Tilbery CP. Characterization of the first symptoms of multiple sclerosis in a Brazilian center: Cross-sectional study . Sao Paulo Med J. 2 017;135(3):222-225. doi:10.1590/1516-3180.2016.0200270117
National MS Society. Vision disorders and multiple sclerosis .
Heitmann H, Biberacher V, Tiemann L et al. Prevalence of neuropathic pain in early multiple sclerosis . Mult Scler. 2016;22(9):1224-30. doi:10.1177/1352458515613643
Tur C. Fatigue management in multiple sclerosis . Curr Treat Options Neurol. 2016;18:26. doi:10.1007/s11940-016-0411-8
Aharony SM, Lam O, Corcos J. Evaluation of lower urinary tract symptoms in multiple sclerosis patients: Review of the literature and current guidelines . Can Urol Assoc J. 2017;11(1-2):61–64. doi:10.5489/cuaj.4058
Walton C, Rechtman L. Rising prevalence of multiple sclerosis worldwide: Insights from the Atlas of MS, third edition . Mult Scler. 2020 Dec; 26(14): 1816–1821. doi:10.1177/1352458520970841
Eccles A. Delayed diagnosis of multiple sclerosis in males: May account for and dispel common understandings of different MS 'types .' Br J Gen Pract. 2019;69(680):148–149. doi:10.3399/bjgp19X701729
Brownlee WJ, Hardy TA, Fazekas F, Miller DH. Diagnosis of multiple sclerosis: Progress and challenges . Lancet . 2017;389(10076):1336-1346. doi:10.1016/S0140-6736(16)30959-X
DiSanto G, Zecca C, MacLachlan S et al. Prodromal symptoms of multiple sclerosis in primary care . Ann Neurol 2018;83(6):1162-1173. doi:10.1002/ana.25247
By Colleen Doherty, MD Dr. Doherty is a board-certified internist and writer living with multiple sclerosis. She is based in Chicago.
- Patient Care & Health Information
- Diseases & Conditions
- Multiple sclerosis
- What is multiple sclerosis? An expert explains
Learn more from neurologist Oliver Tobin, M.B., B.Ch., B.A.O., Ph.D.
I'm Dr. Oliver Tobin, a neurologist specializing in multiple sclerosis at Mayo Clinic. In this video, we'll be covering the basics of multiple sclerosis. What is it? Who gets it? The symptoms, diagnosis, and treatment. Whether you're looking for answers about your own health or that of someone you love, we're here to provide you with the best information available. Multiple sclerosis is a disorder in which the body's immune system attacks the protective covering of the nerve cells in the brain, optic nerve and spinal cord, called the myelin sheath. And this sheath is often compared to the insulation on an electrical wire. When that covering is damaged, it exposes the actual nerve fiber, which can slow or block the signals being transmitted within it. The nerve fibers themselves might also be damaged. The body can repair damage to the myelin sheath, but it's not perfect. The resulting damage leaves lesions or scars, and this is where the name comes from: multiple sclerosis, multiple scars. Now everyone loses brain cells and spinal cord cells as they get older. But if part of the brain or spinal cord has been damaged by MS, the nerve cells in that area will die off faster than the areas around it that are normal. This happens very slowly, usually over decades and typically shows up as gradual walking difficulty happening over several years. When you read about multiple sclerosis, you may hear about different types -- the most frequent being relapsing-remitting multiple sclerosis. And this is characterized by attacks, or relapses.
We don't know what causes MS, but there are certain factors that may increase the risk or trigger its onset. So while MS can occur at any age, it mostly makes its first appearance in people between the ages of 20 and 40. Low levels of vitamin D and low exposure to sunlight, which enables our body to make vitamin D, are associated with an increased risk of developing MS. As people who have MS who have low vitamin D tend to have more severe disease. So people who are overweight are more likely to develop MS and people who have MS and are overweight tend to have more severe disease and a faster onset of progression. People who have MS and who smoke tend to have more relapses, worse progressive disease, and worse cognitive symptoms. Women are up to three times as likely as men to have relapsing-remitting MS. The risk for MS in the general population is about 0.5%. If a parent or sibling has MS, your risk is about twice that or about 1%. Certain infections are also important. A variety of viruses have been linked to MS, including Epstein-Barr virus, which causes mono. Northern and southern latitudes have a higher prevalence, including Canada, the northern US, New Zealand, southeastern Australia, and Europe. White people, especially of northern European descent, are at the highest risk. People of Asian, African, and Native American ancestry have the lowest risk. A slightly increased risk is seen if a patient already has autoimmune thyroid disease, pernicious anemia, psoriasis, type 1 diabetes, or inflammatory bowel disease.
Symptoms of a relapse usually come on over 24 to 48 hours, last for a few days to a few weeks and then improve in the region of 80 to a 100 percent. Those symptoms include loss of vision in an eye, loss of power in an arm or leg or a rising sense of numbness in the legs. Other common symptoms associated with MS include spasms, fatigue, depression, incontinence issues, sexual dysfunction, and walking difficulties.
There's currently no single test to make a diagnosis of MS. However, there are four key features which help to secure the diagnosis. Firstly, are there typical symptoms of multiple sclerosis? Again, those are loss of vision in an eye, loss of power in an arm or leg, or sensory disturbance in an arm or leg lasting for more than 24 hours. Secondly, do you have any physical examination findings consistent with MS? Next, is the MRI of your brain or spine consistent with MS? Now here it's important to note that 95 percent of people over the age of 40 have an abnormal brain MRI, just the same as many of us have wrinkles on our skin. Lastly, are the results of the spinal fluid analysis consistent with MS? Your doctor may recommend blood tests to check for other diseases that share the same symptoms. They may also recommend an OCT test or optical coherence tomography. This is a short scan of the thickness of the layers at the back of your eye.
So the best thing to do when living with MS is to find a trusted interdisciplinary medical team that can help you monitor and manage your health. Having a multidisciplinary team is essential for addressing the individual symptoms that you're experiencing. If you have an MS attack or relapse, your doctor may prescribe you corticosteroids to reduce or improve your symptoms. And if your attack symptoms do not respond to steroids, another option is plasmapheresis or plasma exchange, which is a treatment similar to dialysis. About 50 percent of people who do not respond to steroids have a significant improvement with a short course of plasma exchange. There are over 20 medications currently approved for prevention of MS attacks and prevention of new MRI lesions.
As learning to function with MS can be challenging, there are medical experts ready to work with you to help you manage it, so you can still live a full life. Consulting with a physiatrist, physical or occupational therapist can help you deal with physical difficulties. Physical activity is strongly recommended for all people with MS. Mental health is also an important consideration. So keeping up personal connections with friends and family and trying to stay involved with your hobbies is important. But also be kind to yourself and realistic about what you're up for. This can change from day to day, so it's okay to give yourself permission if something seems like too much or if you need to cancel plans. You may also find support groups helpful to connect with people who understand what you are going through and discuss your feelings and concerns with a doctor or a counselor. Meanwhile, scientists are hard at work, expanding our understanding of this disease and developing new treatments and medications which are ever more effective. If you want to learn more, watch more of our videos or visit mayoclinic.org. We wish you well.
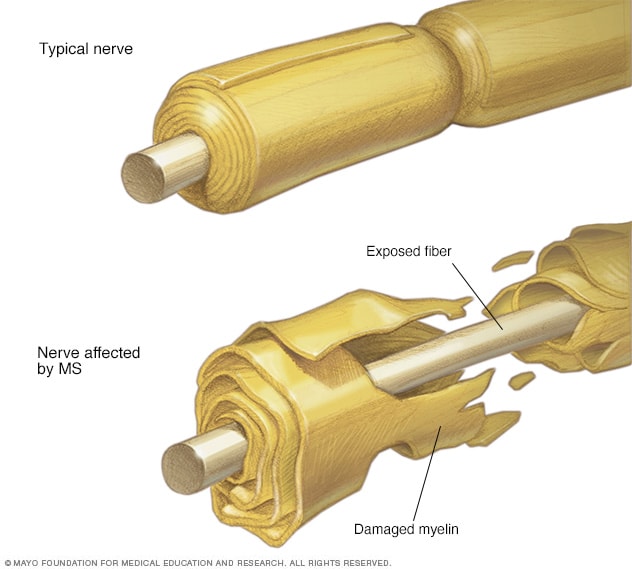
In multiple sclerosis, the protective coating on the nerve fibers is damaged and may eventually be destroyed. This protective coating is called myelin. Depending on where the nerve damage happens, MS can affect vision, sensation, coordination, movement, and bladder or bowel control.
Multiple sclerosis (MS) is a potentially disabling disease of the brain and spinal cord (central nervous system).
In MS , the immune system attacks the protective sheath (myelin) that covers nerve fibers and causes communication problems between your brain and the rest of your body. Eventually, the disease can cause permanent damage or deterioration of the nerve fibers.
Signs and symptoms of MS vary widely between patients and depend on the location and severity of nerve fiber damage in the central nevous system. Some people with severe MS may lose the ability to walk independently or ambulate at all. Other individuals may experience long periods of remission without any new symptoms depending on the type of MS they have.
There's no cure for multiple sclerosis. However, there are treatments to help speed the recovery from attacks, modify the course of the disease and manage symptoms.

Products & Services
- A Book: Mayo Clinic Family Health Book
- Newsletter: Mayo Clinic Health Letter — Digital Edition
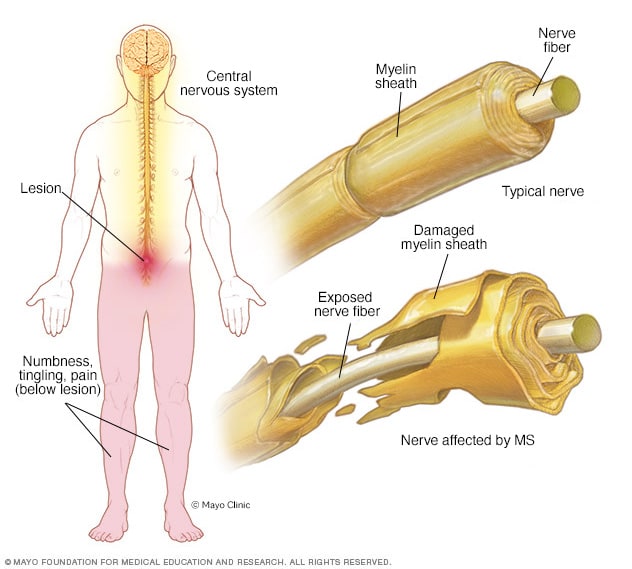
- Myelin damage and the nervous system
In multiple sclerosis, the protective coating on nerve fibers, known as myelin, in the central nervous system is damaged. Depending on the location of the damage in the central nervous system, symptoms may happen, including numbness, tingling, weakness, visual changes, bladder and bowel troubles, memory troubles, or mood changes, for example.
Multiple sclerosis signs and symptoms may differ greatly from person to person and over the course of the disease depending on the location of affected nerve fibers.
Common symptoms include:
- Numbness or weakness in one or more limbs that typically occurs on one side of your body at a time
- Electric-shock sensations that occur with certain neck movements, especially bending the neck forward (Lhermitte sign)
- Lack of coordination
- Unsteady gait or inability to walk
- Partial or complete loss of vision, usually in one eye at a time, often with pain during eye movement
- Prolonged double vision
- Blurry vision
- Problems with sexual, bowel and bladder function
- Slurred speech
- Cognitive problems
- Mood disturbances
When to see a doctor
See a doctor if you experience any of the above symptoms for unknown reasons.
Disease course
Most people with MS have a relapsing-remitting disease course. They experience periods of new symptoms or relapses that develop over days or weeks and usually improve partially or completely. These relapses are followed by quiet periods of disease remission that can last months or even years.
Small increases in body temperature can temporarily worsen signs and symptoms of MS . These aren't considered true disease relapses but pseudorelapses.
At least 20% to 40% of those with relapsing-remitting MS can eventually develop a steady progression of symptoms, with or without periods of remission, within 10 to 20 years from disease onset. This is known as secondary-progressive MS .
The worsening of symptoms usually includes problems with mobility and gait. The rate of disease progression varies greatly among people with secondary-progressive MS .
Some people with MS experience a gradual onset and steady progression of signs and symptoms without any relapses, known as primary-progressive MS .
More Information
Multiple sclerosis care at Mayo Clinic
- Multiple sclerosis: Can it cause seizures?
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
The cause of multiple sclerosis is unknown. It's considered an immune mediated disease in which the body's immune system attacks its own tissues. In the case of MS , this immune system malfunction destroys the fatty substance that coats and protects nerve fibers in the brain and spinal cord (myelin).
Myelin can be compared to the insulation coating on electrical wires. When the protective myelin is damaged and the nerve fiber is exposed, the messages that travel along that nerve fiber may be slowed or blocked.
It isn't clear why MS develops in some people and not others. A combination of genetics and environmental factors appears to be responsible.
Risk factors
These factors may increase your risk of developing multiple sclerosis:
- Age. MS can occur at any age, but onset usually occurs around 20 and 40 years of age. However, younger and older people can be affected.
- Sex. Women are more than 2 to 3 times as likely as men are to have relapsing-remitting MS .
- Family history. If one of your parents or siblings has had MS , you are at higher risk of developing the disease.
- Certain infections. A variety of viruses have been linked to MS , including Epstein-Barr, the virus that causes infectious mononucleosis.
- Race. White people, particularly those of Northern European descent, are at highest risk of developing MS . People of Asian, African or Native American descent have the lowest risk. A recent study suggests that the number of Black and Hispanic young adults with multiple sclerosis may be greater than previously thought.
- Climate. MS is far more common in countries with temperate climates, including Canada, the northern United States, New Zealand, southeastern Australia and Europe. Your birth month may also affect the chances of developing multiple sclerosis, since exposure to the sun when a mother is pregnant seems to decrease later development of multiple sclerosis in these children.
- Vitamin D. Having low levels of vitamin D and low exposure to sunlight is associated with a greater risk of MS .
- Your genes. A gene on chromosome 6p21 has been found to be associated with multiple sclerosis.
- Obesity. An association with obesity and multiple sclerosis has been found in females. This is especially true for female childhood and adolescent obesity.
- Certain autoimmune diseases. You have a slightly higher risk of developing MS if you have other autoimmune disorders such as thyroid disease, pernicious anemia, psoriasis, type 1 diabetes or inflammatory bowel disease.
- Smoking. Smokers who experience an initial symptom that may signal MS are more likely than nonsmokers to develop a second event that confirms relapsing-remitting MS .
Complications
People with multiple sclerosis may also develop:
- Muscle stiffness or spasms
- Severe weakness or paralysis, typically in the legs
- Problems with bladder, bowel or sexual function
- Cognitive problems, like forgetfulness or word finding difficulties
- Mood problems, such as depression, anxiety or mood swings
- Seizures, though very rare
- What is multiple sclerosis? National Multiple Sclerosis Society. https://www.nationalmssociety.org/What-is-MS. Accessed June 2, 2022.
- Daroff RB, et al. Multiple sclerosis and other inflammatory demyelinating diseases of the central nervous system. In: Bradley's Neurology in Clinical Practice. 7th ed. Philadelphia, Pa.: Elsevier Saunders; 2012. https://www.clinicalkey.com. Accessed June 2, 2022.
- Ferri FF. Multiple sclerosis. In: Ferri's Clinical Advisor 2019. Philadelphia, Pa.: Elsevier; 2019. https://www.clinicalkey.com. Accessed June 2, 2022.
- Olek MJ. Clinical presentation, course, and prognosis of multiple sclerosis in adults. https://www.uptodate.com/contents/search. Accessed June 2, 2022.
- Wingerchuk DM (expert opinion). Mayo Clinic, Phoenix/Scottsdale, Ariz. Jan. 21, 2019.
- Ciccarelli O. Multiple sclerosis in 2018: New therapies and biomarkers. The Lancet. 2019; doi: 10.1016/S14744422 (18)30455-1.
- Keegan BM. Therapeutic decision making in a new drug era in multiple sclerosis. Seminars in Neurology. 2013; doi:10.1055/s0033-1345709.
- Goldman L, et al., eds. Multiple sclerosis and demyelinating conditions of the central nervous system. In: Goldman-Cecil Medicine. 25th ed. Philadelphia, Pa.: Saunders Elsevier; 2016. https://www.clinicalkey.com. Accessed Jun. 2, 2022.
- Lotze TE. Pathogenesis, clinical features, and diagnosis of pediatric multiple sclerosis. https://www.uptodate.com/contents/search. Accessed June 2, 2022.
- Kantarci OH, et al. Novel immunomodulatory approaches for the management of multiple sclerosis. Clinical Pharmacology & Therapeutics. 2014; doi:10.1038/clpt.2013.196.
- Olek MJ. Disease-modifying treatment of relapsing-remitting multiple sclerosis in adults. https://www.uptodate.com/contents/search. Accessed June 2, 2022.
- Olek MJ, et al. Treatment of acute exacerbations of multiple sclerosis in adults. https://www.uptodate.com/contents/search. Accessed June 2, 2022.
- Wingerchuk DM. Multiple sclerosis: Current and emerging disease-modifying therapies and treatment strategies. Mayo Clinic Proceedings. 2014; doi:10.1016/j.mayocp.2013.11.002.
- Pizzorno JE, et al. Multiple sclerosis. In: Textbook of Natural Medicine. 4th ed. St. Louis, Mo.: Churchill Livingstone Elsevier; 2013. https://www.clinicalkey.com. Accessed June 2, 2022.
- Olek MJ, et al. Evaluation and diagnosis of multiple sclerosis in adults. https://www.uptodate.com/contents/search. Accessed June 2, 2022.
- Gaetani L, et al. 2017 revisions of McDonald criteria shorten the time to diagnosis of multiple sclerosis in clinically isolated syndromes. Journal of Neurology. 2018;265:2684.
- http://onlinelibrary.wiley.com/doi/10.1002/ana.22366.
- Olek MJ, et al. Pathogenesis and epidemiology of multiple sclerosis.
- Ingram G, et al. Cannabis and multiple sclerosis. Practical Neurology. 2019; doi:10.1136/practneurol-2018-002137.
- Olek MJ, et al. Symptom management of multiple sclerosis in adults. https://www.uptodate.com/contents/search. Accessed June 2, 2022.
- Yadav Y, et al. Summary of evidence-based guideline: Complementary and alternative medicine in multiple sclerosis. Neurology. 2014; doi: 10.1212/WNL.0000000000000250.
- Nimmagadda R. Allscripts EPSi. Mayo Clinic. April 22, 2022.
- National MS Society. Network of Pediatric MS Centers. https://www.nationalmssociety.org/What-is-MS/Who-Gets-MS/Pediatric-MS/Care-for-Pediatric-MS. Accessed June 2, 2022.
- Rodriguez M. Plasmapheresis in acute episodes of fulminant CNS inflammatory demyelination. Neurology. 1993; doi:10.1212/wnl.43.6.1100.
- Deb C. CD8+ T cells cause disability and axon loss in a mouse model of multiple sclerosis. PLoS One. 2010; doi:101371/journal.pone.0012478.
- FDA approves new drug to treat multiple sclerosis. U.S. Food & Drug Administration. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm549325.htm. Accessed June 1, 2022.
- Keegan BM (expert opinion). Mayo Clinic, Rochester, Minn. January 15, 2019.
- FDA approves new oral drug to treat multiple sclerosis. U.S. Food and Drug Administration. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm634469.htm. Accessed June 2, 2022.
- Kappos L, et al. Siponimod versus placebo in secondary progressive multiple sclerosis (EXPAND): A double-blind, randomized, phase 3 study. The Lancet. 2018; doi: 10.1016/S0140-6736(18)30475-6.
- Marin Collazo IV (expert opinion). Mayo Clinic, Rochester, Minn. April 2, 2019.
- AskMayoExpert. Multiple sclerosis. Mayo Clinic; 2020.
- AskMayoExpert. Medication monitoring guidelines. Mayo Clinic; 2020.
- Vumerity. National MS Society. https://www.nationalmssociety.org/Treating-MS/Medications/Vumerity. Accessed March 16, 2020.
- Gianfrancesco M, et al. Obesity during childhood and adolescence increases susceptibility to multiple sclerosis after accounting for established genetic and environmental risk factors. Obesity Research and Clinical Practice. 2014; doi.org/10.1016/j.orcp.2014.01.002.
- Pantavou KG, et al. Season of birth and multiple sclerosis: A systematic review and multivariate meta-analysis. Journal of Neurology. 2020; doi:10.1007/s00415019-09346-5.
- Cifu DX, et al., eds. Multiple sclerosis. In Braddom's Physical Medicine and Rehabilitation. 6th ed. Elsevier; 2021 https://www.clinicalkey.com. Accessed Jun. 2, 2022.
- Langer-Gould AM, et al. Racial and ethnic disparities in multiple sclerosis prevalence. Neurology. 2022; doi:10.1212/WNL.0000000000200151.
- Kasper LH, et al. Immunomodulatory activity of interferon-beta. Annals of Clinical and Translational Neurology. 2014; doi:10.1002/acn3.84.
- Goldschmidt CH, et al. Re-evaluating the use of IFN-B and relapsing multiple sclerosis: Safety, efficacy and place in therapy. Degenerative Neurological and Neuromuscular Disease. 2020; doi:10.2147/DNND.S224912.
- Kieseie BC. The mechanism of action of interferon-B in relapsing multiple sclerosis. Central Nervous System Drugs. 2011; doi:10.1007/s10067-008-0972-3.
- Betaseron. Bayer AG; 1993. www.bayer.com. Accessed Jun. 1, 2022.
- Hauser SL, et al. Ofatumumab versus teriflunomide in multiple sclerosis. The New England Journal of Medicine. 2020; doi:10.1056/NEJMoa1917246.
- Kesimpta. Novartis; 2020. www.novartis.com. Accessed Jun. 1, 2022.
- Marin Collazo V (expert opinion). Mayo Clinic. June 13, 2020.
- Olek MJ. Treatment of progressive multiple sclerosis in adults. https://www.uptodate.com/contents/search. Accessed Jun. 2, 2022.
- Wingerchuk DM, et al. Disease modifying therapies for relapsing multiple sclerosis. British Medical Journal. 2016; doi:10.1136/bmj.i3518.
- Saadeh RS, et al. CSF kappa free light chains: Cutoff validation for diagnosing multiple sclerosis. Mayo Clinic Proceedings. 2022; doi:10.1016/j.mayocp.2021.09.014.
- Goldschmidt C, et al. Advances in the treatment of multiple sclerosis. Neurologic Clinics. 2021; doi:10.1016/j.ncl.2020.09.002.
- Bafiertam. Banner Life Sciences LLC; 2013. www.bannerls.com. Accessed Jun. 1, 2022.
- Baliertam delayed release capsule. Banner Life Sciences LLC; 2013. www.bannerls.com. Accessed Jun. 1, 2022.
- Oral ponesimod versus teriflunomide in relapsing multiple sclerosis (OPTIMUM). ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT02425644. Accessed Jun. 2, 2022.
- Ponvory. Janssen Pharmaceuticals; 2021. www.janssen.com. Accessed Jun. 1, 2022.
- Torke S, et al. Inhibition of Bruton's tyrosine kinase as a novel therapeutic approach in multiple sclerosis. Expert Opinion on Investigational Drugs. 2020.
- Nash RA, et al. High-dose immunosuppressive therapy and autologous hematopoietic cell transplantation for relapsing-remitting multiple sclerosis (HALT-MS): A 3-year interim report. Journal of the American Medical Association Neurology. 2015; doi:10.1001/jamaneurol.2014.3780.
- Reston, et al. Autologous hematopoietic cell transplantation for multiple sclerosis: A systematic review. Multiple Sclerosis. 2011; doi:10,1177/1352458510383609.
- Petrou P, et al. Beneficial effects of autologous mesenchymal stem cell transplantation in active progressive multiple sclerosis. Brain. 2020; doi:10.1093/brain/awaa333.
- Liang J, et al. Allogenic mesenchymal stem cell transplantation in the treatment of multiple sclerosis. Multiple Sclerosis. 2009; doi:10.1177/1352458509104590.
- Wingerchuk DM, et al. Multiple sclerosis: Current and emerging disease-modifying therapies and treatment strategies. Mayo Clinic Proceedings. 2014; doi:101016/j.mayocp.2013.11.002.
- Multiple sclerosis information page. National institute of neurological disorders and stroke. https://www.ninds.nih.gov/Disorders/All-Disorders/Multiple-Sclerosis-Information-Page. Accessed Jun. 2, 2022.
- Sadovnick AD. Genetic background of multiple sclerosis. Autoimmunity Reviews. 2012; doi:10.1016/j.autrev.2011.05.007.
- Acetyl-L-carnitine: Can it relieve MS fatigue?
- Demyelinating disease: What can you do about it?
- Emerging treatments for multiple sclerosis
- Exercise and multiple sclerosis
- Explaining multiple sclerosis
- Infographic: Multiple Sclerosis
- MRI multiple sclerosis lesions
- Multiple sclerosis FAQs
- Physical therapy for multiple sclerosis
- Vitamin D and MS: Any connection?
- Vitamins for MS: Do supplements make a difference?
Associated Procedures
- Lumbar puncture (spinal tap)
Mayo Clinic in Rochester, Minnesota, Mayo Clinic in Phoenix/Scottsdale, Arizona, and Mayo Clinic in Jacksonville, Florida, have been ranked among the best Neurology & Neurosurgery hospitals in the nation for 2024-2025 by U.S. News & World Report.
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- NEW: Listen to Health Matters Podcast - Mayo Clinic Press NEW: Listen to Health Matters Podcast
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Thank a researcher today
Their crucial work saves lives every day. Let Mayo Clinic researchers know they’re appreciated with a quick message.
- Skip to content
- Accessibility help
Multiple sclerosis: When should I suspect that a person has multiple sclerosis?
Last revised in May 2024
When should I suspect that a person has multiple sclerosis?
- About 0.5% of adults with MS first develop symptoms aged 60 years or older — older age at onset is associated with a progressive course.
- A history of previous neurological symptoms.
- Symptoms that evolve over more than 24 hours, may persist over several days or weeks and then improve.
- Loss or reduction of vision in one eye with painful eye movements.
- Ascending sensory disturbance and/or weakness.
- Balance or gait problems, unsteadiness, or clumsiness.
- Altered sensation radiating down the back and sometimes into the limbs on neck flexion (Lhermitte's symptom).
- Optic neuritis is the initial presentation in about 20–30% of people with MS.
- The person may describe partial or total unilateral visual loss developing over a few days, pain behind the eye (in particular on eye movement) and/or loss of colour discrimination (particularly reds).
- Fundoscopy is often normal but the disc may appear pale or swollen. There may be paradoxical dilation of the pupil when light is rapidly shifted from the unaffected eye to the affected eye (relative afferent pupillary defect).
- Optic neuritis may be bilateral, but if this occurs extra vigilance is needed to rule out neuromyelitis optica which is often confused with MS and needs urgent treatment.
- May present with sensory symptoms (such as paraesthesia) or motor symptoms (such as weakness) below the level of the inflammation that typically develop over hours or days.
- Some people describe a tight band sensation around the trunk at the level of the inflammation, or a shock-like sensation radiating down the spine induced by neck flexion (Lhermitte’s phenomena).
- There may be urinary symptoms such as urgency, frequency, or retention.
- Examination may reveal focal muscle weakness and reduced sensation below the affected spinal level. Muscle tone is initially reduced.
- Symptoms and signs may be symmetrical or asymmetrical, and tend to reflect a partial myelitis that only affects a part of the spinal cord — symptoms and signs similar to a full spinal cord transection are rare.
- These may include ataxia, vertigo, clumsiness, and dysmetria (as demonstrated by abnormalities with finger-to-nose testing and walking heel to toe).
- Eye movement abnormalities that can cause diplopia, oscillopsia (a sensation of movement of the vision), nystagmus, and internuclear ophthalmoplegia (inability to adduct one eye and nystagmus in the abducting eye on oculomotor examination).
- Bulbar muscle problems resulting in dysarthria or dysphagia.
- The person's main symptoms are fatigue, depression, or dizziness unless they have a history or evidence of focal neurological symptoms or signs.
Basis for recommendation
The information on the possible presentations of multiple sclerosis is based on the National Institute for Health and Care Excellence (NICE) guideline Multiple sclerosis in adults: management [ NICE, 2022 ] and expert opinion in review articles [ Reich, 2018 ; Thompson, 2018 ; Wallin, 2019 ; BMJ Best Practice, 2021 ].
The content on the NICE Clinical Knowledge Summaries site (CKS) is the copyright of Clarity Informatics Limited (trading as Agilio Software Primary Care) . By using CKS, you agree to the licence set out in the CKS End User Licence Agreement .

IMAGES
VIDEO
COMMENTS
Two phenomena—clinically isolated syndrome and optic neuritis—may serve as early warning signs of MS. People who experience one (or both) of these may or may not go on to develop MS.…
Presentation of MS often varies among patients. Some patients have a predominance of cognitive changes, while others present with prominent ataxia, hemiparesis or paraparesis, …
Optic neuritis, which is usually monocular, can be the first sign of MS. Fundoscopy may reveal blurring of the optic disc in the acute setting, though often no changes are apparent. A previous episode of optic neuritis is often …
The early signs and symptoms of MS can be the same for women and men. One of the more obvious first signs of MS is a problem with vision, known as optic neuritis. This is often because it's a more concrete symptom as opposed to …
We don't know what causes MS, but there are certain factors that may increase the risk or trigger its onset. So while MS can occur at any age, it mostly makes its first appearance in people between the ages of 20 and 40.
Optic neuritis is the initial presentation in about 20–30% of people with MS. The person may describe partial or total unilateral visual loss developing over a few days, pain behind the eye …
People with multiple sclerosis (MS) tend to have their first symptoms between the ages of 20 and 40. Early on, the symptoms get better, but then they come back. This is called...
Multiple sclerosis (MS) affects function in cognitive, emotional, motor, sensory, or visual areas and occurs as a result of a person’s immune system attacking their brain and spinal cord. It is estimated that over 1.8 million …